Cancer: “The Forgotten C” of the Pandemic

![]() Cancer- “The Forgotten C” of the Pandemic
Cancer- “The Forgotten C” of the Pandemic

With Victorian health department and government officials focused entirely on COVID-19 case numbers, and people afraid to go to doctor’s rooms and hospitals, for fear of catching the disease, cancer specialists such as myself see a new emerging public health crisis going unnoticed, which may lead to more avoidable deaths from cancer than from coronavirus itself
Significant reductions in 5 and 10 year breast cancer survival due to delays in diagnosis and treatment occurring as a result of the extreme and extended Victorian pandemic restrictions threaten to potentially negate the hard won improvements in breast cancer mortality achieved over the last 20 years.
A significant reduction in the number of new breast cancer diagnoses has been reported both nationally and internationally during the pandemic. This is likely to be related to both the reluctance of patients to attend medical facilities for the investigation of breast symptoms, and also the temporary suspension and subsequent reduction in activity of population breast screening programmes.
What has become clear is that people aren’t coming forward with signs or symptoms that could be cancer. It’s not particularly surprising, as many are giving health services a wide berth at this time. But cancer doesn’t stop just because we’re in a coronavirus pandemic, and early diagnosis is as important as it’s ever been.
Delays in diagnosing and treating people with cancer could potentially lead to more years of lost life than with Covid-19, and modellers in the UK estimate the excess of cancer deaths is going to be way greater than from Covid-19. This excess is likely to be even more marked here in Australia, where we have experienced fewer COVID related deaths than in the United Kingdom, and in fact, unlike in many other countries, have not experienced an excess in overall deaths in 2020.
There are highly likely to be more overall deaths, and inevitably more “life years” lost because of delayed cancer diagnoses than from coronavirus. The “life year” loss is much, much greater from cancer deaths, because of the advanced average age of COVID fatalities in comparison to cancer deaths. As cancer patients are generally younger than COVID associated fatalities, the predicted “years of lost life may be quite dramatic” on top of “a huge amount of avoidable mortality”.
To provide some context, in a state of 6.6 million people, there are currently, as of 12.9.20, only 126 patients hospitalised with COVID in Victoria, 9 of whom are in ICU.
Over 5000 Victorian women would be expected under normal circumstances to be diagnosed with breast cancer every year, however this number is likely to be much lower in 2020 because of the significant fall in breast cancer diagnoses reported as a result of pandemic restrictions. Delays of over 3 months may be associated with a reduction in survival, and ignoring life-threatening non–COVID-19 conditions such as cancer for too long during the pandemic runs the real risk of turning one public health crisis into many others. As weeks have now turned to months, a troubling trend has emerged: a precipitous drop in cancer diagnoses. Experts fear that with each passing day, the prognosis for some of those undiagnosed cases may be getting worse, as potential patients huddle at home.
The consequences for cancer outcomes could be substantial. For cancer patients, the unintended consequences start with those who don’t even know they have the disease yet. In general, the earlier one receives cancer treatment, the better the results. A delayed diagnosis may result in a breast cancer being diagnosed at a later stage – with an increased likelihood of more extensive surgery, radiotherapy and chemotherapy, as well as, possibly, a poorer outcome.
There has been a steep drop in breast cancer diagnoses reported internationally, nationally and locally since the start of the pandemic, but there is no reason to believe the incidence of cancer has dropped. Cancers being missed now, will still come to light eventually, but at a later stage (“upstaging”) and with worse prognoses. Ultimately, people diagnosed at a later stage will have a higher risk of not being cured from their cancer.
Why is the general public not more alarmed about this situation?
The simple answer is that most people are unaware of the seriousness of the unintended consequences of the restrictions, which were initially introduced with the justification that they were essential to help manage limited health care resources.
The authorities are so single-mindedly focused on COVID case numbers that other health conditions are being ignored, and clinicians and specialists who are critical of the government pandemic response and attempt to advocate for non COVID related conditions are often met with incorrect accusations of “politicising” by ill-informed sections of the community who have been brainwashed by the very limited amount of information and data released by the department of health.
Cancer diagnostics and the instigation of treatment have been disrupted by the pandemic response. As Victorian authorities persist with a pandemic response policy focused entirely on the reduction of COVID case numbers, to the exclusion of all else, the progression of cancers during the resulting delay will inevitably have an impact on patients’ long-term survival.
Fear of contracting the coronavirus in health care settings has dissuaded people from screening, diagnosis, and treatment for non–COVID-19 diseases. Patients are frightened, especially older patients and those with existing health conditions. Many are shielding by minimising interactions between themselves and others and staying home as much as possible, and are strongly encouraged by authorities to do so. Continued travel restrictions and fear of infection play a major part, and in addition many would-be patients aren’t setting up appointments because they don’t know they need to.

General practices remain open and cancer specialists continue to conduct in office, face-to-face consultations for patients with suspected or proven cancer, however public health warnings have been deliberately calibrated by authorities to strongly emphasise the danger of COVID to sections of the community they perceive as more “risk -taking” and potentially reckless, such as the young, resulting in the more timorous being in a constant state of unnecessary terror and therefore reluctant to leave their homes to seek medical attention.
The number of breast cancer screenings plummeted when initial lockdowns went into effect, (by an estimated 94% in the USA) meaning many of the people who would be seeking care don’t yet know they have cancer at all. For cancer patients, the unintended consequences start with those who don’t even know they have the disease yet.
Six months in, we continue in Melbourne to have the most extreme global lockdown in place, and with the procedures put in place in health facilities to ensure the safety of our patients and our staff, the potential health impact from cancer is a bigger concern than the pandemic.
New cancer diagnoses in the USA fell during the COVID-19 pandemic, according to a study in JAMA Network Open. Compared with the baseline period (January and February), weekly diagnoses of breast cancer fell 52% for the period March 1 to April 18, 2020.
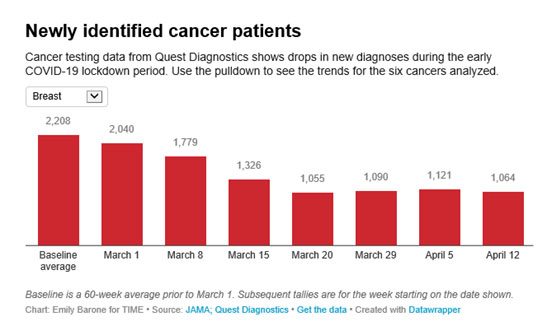
Kaufman et al, JAMA Network, 2020
The Netherlands Cancer Registry has seen as much as a 40% decline in weekly cancer incidence, and the United Kingdom has experienced a 75% decline in referrals for suspected cancer since COVID-19 restrictions were implemented.
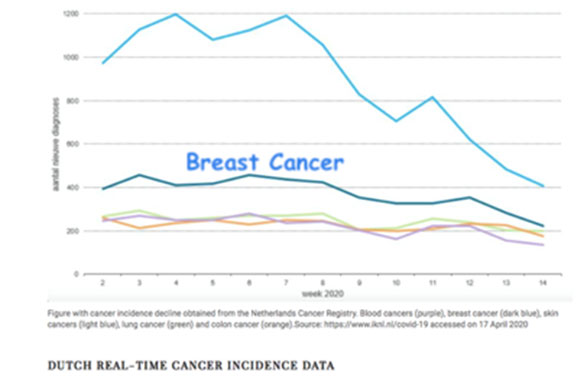
Here in Victoria, data from the Victorian Cancer Registry at Cancer Council Victoria, revealed that from April through to mid-May 2020 there was a reduction of up to 37 per cent in breast cancer reporting.
As a Specialist Oncoplastic Breast Cancer Surgeon, more than 90% of my practice is devoted to breast cancer surgery, and I can personally report a significant reduction in new breast cancer diagnoses since the onset of the pandemic. New breast cancer referrals for the 6 month period 16.3.20-12.9.20 are down 40% compared with the same period in 2019 and 41% compared to 2018. The magnitude of the fall has increased during the second lockdown with new breast cancer diagnoses June 15 – Sept 12 down by 70% on both 2018 and 2019.
For patients with cancer, delay of surgery has the real potential to increase the likelihood of metastatic disease, with some patients’ tumours progressing from being curable (with near-normal life expectancy) to non-curable (with limited life expectancy).
What will be the likely impact of the pandemic on cancer mortality ?
American modelling of the effect of COVID-19 on cancer screening and treatment for breast cancer over the next decade suggests an increase in deaths. The number of excess deaths per year would peak in the next year or two. Ignoring life-threatening non– COVID-19 conditions such as cancer for too long may turn one public health crisis into many others.
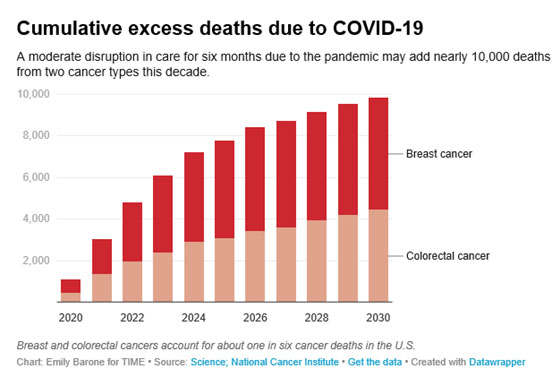
Sharpless, Science, 2020
Delays in cancer referrals caused by the COVID-19 pandemic and the ensuing shutdown in cancer services will lead to thousands of additional deaths and tens of thousands of life-years lost, suggest two new modelling studies from the United Kingdom, published in Lancet Oncology in July 2020. The investigators used population based modelling data to estimate the impact of diagnostic delays resulting from 12 months of physical distancing. For breast cancer, this would lead to a 7.9% to 9.6% increase in the number of cancer deaths within 5 years after diagnosis.
Many of these will be young or middle-aged people, and on average, those who die would have lived for 20 more years if their cancers had been identified promptly, without the delay caused by the coronavirus pandemic.
These estimates paint a sobering picture and reflect the many young people who are affected by cancer in the prime of life, during their most productive years. The researchers are calling for media campaigns to make people aware that the risk of death from cancer by delaying diagnosis may for many people significantly outweighs the risk of dying from Covid-19.
The estimated reduction in 5 and 10 year breast cancer survival is dependent on the magnitude of delay (3 vs 6 month delay), the age of the patient, the stage of the cancer and the pathological subtype. In many instances, the reduction in survival is of the same order of magnitude as the gain one would potentially expect from undergoing adjuvant chemotherapy, and is therefore a significant negative outcome for the patient.
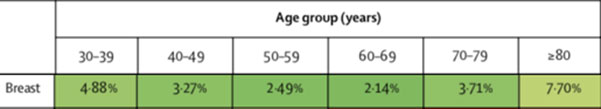
Reduction in 10-year net survival in England incurred from a 3-month delay, by age group
Sud et al, Lancet Oncology, 2020
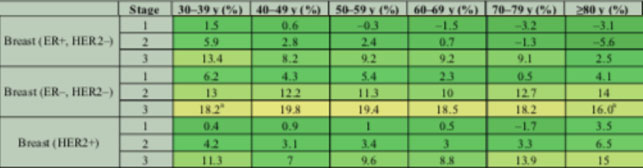
Reduction in 5-year net survival as a consequence of 6-month delay to surgery by breast cancer stage and age of diagnosis in England
Sud et al, Annals of Oncology, 2020
Don’t delay your medical care. It sounds like common sense, but in the era of COVID-19, people who normally wouldn’t hesitate to call a doctor when something doesn’t feel right, might avoid doing so out of concern about any kind of lockdown activity. But the medical community is urgently trying to advise the public that seeking health care is still essential.
Cancer does not wait for the pandemic, and it is very important that the public receive the consistent message that anyone who is experiencing any concerning breast symptoms reach out to their GP for immediate evaluation, followed by timely onward specialist referral if appropriate.
It is equally, if not more important, that authorities revisit their single minded focus on reducing COVID case numbers. A COVID-19 response is not complete without identifying and mitigating the unintended consequences that pandemic strategies will have on public health. In the midst of a pandemic, we cannot and should not abandon the prevention and management of other diseases.
While this is a concern across all fields of medicine, it is particularly vital in cancer care, where early detection is key. The prognosis for cancer patients almost always depends on how advanced the disease is at diagnosis. The more the cancer has grown or spread, the more difficult it is to treat, and the worse patients generally fare.
Another factor is that any significant delay in cancer diagnosis would hide from the immediate numbers researchers use to analyze the impact of the phenomenon, since cancer mortality is measured in years, compared to traumatic events like a heart attack. It may be that rather than dying in several years, you die in one year instead. The effects of delaying cancer diagnoses are something we’ll be dealing with for a long time.
The excessive and extended restrictions imposed on the Victorian people should be relaxed as soon as possible in order to minimise the unintended consequences of the extreme lockdown and to reduce the collateral damage inflicted on cancer outcomes over years to come.
Failure to prevent and manage other medical conditions will lead to other prolonged public health crises long after COVID-19 is contained. Cancer deaths could even go back up to levels we haven’t seen for years in Australia. We have to work this out because despite what the authorities would have us believe, the virus will be with us for a while, and cancer is definitely not going anywhere.
References:
![]() Collateral damage: the impact on outcomes from cancer surgery of the
Collateral damage: the impact on outcomes from cancer surgery of the
COVID-19 pandemic
![]() The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England
The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England











