Lumpectomy vs Mastectomy: How to Choose

Lumpectomy vs. Mastectomy: How to Choose
Women who’ve been recently diagnosed with breast cancer are almost immediately faced with treatment choices. Irrespective of the sequencing of treatment modalities for early breast cancer, surgery forms an integral part, for both invasive and preinvasive breast malignancy (DCIS).
Resources and general information on the treatment of breast cancer, including breast surgery, can be found in in electronic format on the website www.thebreastcentre.com.au: Before Your Consultation with the Breast Surgeon
This section deals in more detail with the advantages and disadvantages of the two main types of breast cancer surgery, and factors which may help you choose between the two, if both are options in your case.
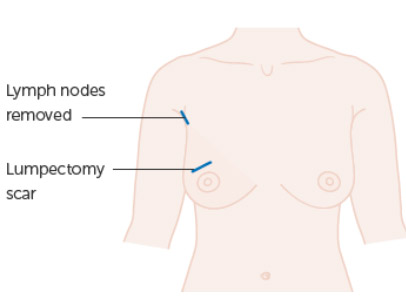
- Breast conserving surgery (BCS) -also called lumpectomy or wide local excision (WLE) This involves the removal of the part of the breast affected by the cancer, together with a small margin of surrounding normal breast tissue. When combined with post-operative radiotherapy, the term used is breast conserving therapy (BCT).
- Mastectomy. This involves the total removal of one or both breasts. See Types of Mastectomy
In most cases, surgery for invasive breast cancer also involves the removal of some lymph nodes from the armpit (axilla). See Sentinel Node Biopsy
Before jumping into the discussion of the two surgical therapies, I want to make one point very clear: for early stage breast cancer, there is absolutely NO difference in survival between a mastectomy and a lumpectomy with radiation. Let me repeat that so it can sink in: for early stage breast cancer, there is absolutely no difference in survival between a mastectomy and a lumpectomy with radiation. There are other differences between these two therapies and one choice is not better than the other. It just depends on what’s right for you.
As part of your early breast cancer treatment, you may be able to choose between a mastectomy or a lumpectomy with radiation. You may also wish that someone would just decide for you.
Are you worrying about making the wrong choice? Are you wondering if you’ll be second-guessing your decision should the cancer return in the future? Are your thoughts consumed with just getting the cancer out of your body by whatever means possible? These reactions and concerns are normal, but they still make the decision difficult.
Fortunately, there is no wrong decision.

There have been six randomized trials comparing breast conserving surgery and mastectomy, which found no survival advantage for either surgery option. In 1990, the American National Cancer Institute (NCI) consensus panel came to the conclusion that breast-conserving surgery was the optimal treatment based on these trials. Since that time, the trend in surgery choice has shifted, with breast-conserving surgery initially rising, but then declining since 2006, as mastectomy rates have increased, and what is largely driving the increase in mastectomy rates, is bilateral mastectomies.
Studies show that women with early stage breast cancer who have breast-conserving surgery followed by radiation therapy have the same survival rates as women who have a mastectomy. This means that your doctor will give you a choice between the two operations if there isn’t a medical reason for you to have one rather than the other.
The choice between breast-conserving surgery and mastectomy is a very personal one. In addition, it comes at a time that is emotionally charged. Your feelings, preferences, priorities and lifestyle all play a part in your decision. You may choose to have breast-conserving surgery because you want to keep as much of your breast as possible. Or having a mastectomy may give you better peace of mind because it removes more breast tissue.

First, talk with your breast surgeon to see if you have a choice between mastectomy and lumpectomy plus radiation therapy. Some women may not have a choice, as oncologically the only appropriate surgical option for them is mastectomy. Approximately 25% of women will require mastectomy, but for the remaining 75%, there is a choice.
- The& size of thecancer in relation to the size of the breast is usually the main factor that a breast surgeon considers to determine if lumpectomy is an appropriate surgical treatment option to consider. Whether lumpectomy is a realistic possibility, is related to the % volume of the breast which requires excision to remove the cancer with adequate pathological margins, in comparison to the overall size of the breast, also taking into account where the tumour lies within the breast, as some areas of the breast are more cosmetically sensitive to volume loss than others.
- In some instances, especially if you have a large tumour or proven lymph node involvement, chemotherapy or hormone therapy may be recommended before you have surgery. This will help to shrink the tumour before breast cancer surgery, and is called “neoadjuvant” therapy.

The decision to offer a lumpectomy as an option to the patient is therefore largely driven by the size of the tumour in relation to the size of the breast. If it is felt that the cosmetic result following lumpectomy and radiation would be acceptable, lumpectomy is usually offered as an option.
Larger % volumes can potentially be removed whilst still achieving good cosmesis with the use of oncoplastic techniques. Oncoplastic breast cancer surgery uses plastic surgical techniques to redistribute volume loss. Integrating oncoplastic techniques into breast conservation may potentially allow wider excision of larger volumes of breast tissue, thereby expanding the limits of breast conservation. See Oncoplastic Breast Surgery

A mastectomy may be the best surgical option when:
- There are two or more tumours (multi-centric tumours) in different quadrants of your breast that cannot be removed with a single wide excision
- The tumour is large (relative to breast size). In some cases, chemotherapy before surgery (neoadjuvant therapy) can shrink large cancers to enable breast conservation (lumpectomy) where mastectomy would otherwise have been required.
- The mammogram is diffusely abnormal, for example when there are extensive areas of suspicious calcifications in the breast, which can be associated with widespread preinvasive disease (DCIS). It is important to appreciate that the requirement for more radical/extensive breast surgery, ie mastectomy, does not necessarily bear a direct relationship to prognosis. A mastectomy may be required for widespread preinvasive disease, which has an excellent prognosis following surgery, and yet an aggressive, high grade invasive carcinoma, which has spread to lymph nodes, may be successfully treated with breast conserving surgery.
- The surgeon cannot achieve clear/negative pathological margins (remove all the tumour) despite attempt(s) at lumpectomy.

- Genetic predisposition: Some women with a genetic predisposition to develop breast cancer opt for bilateral mastectomy—removal of both breasts—as a preventive measure after developing cancer in one breast. In women with the BRCA1 /BRCA2 or some of the other gene mutations, the chances of developing breast cancer can be as high as 70-80%. Having developed a breast cancer, the chances of developing another primary breast cancer in any remaining breast tissue is also high. Many therefore choose double mastectomy. Patients in their 20s and 30s sometimes also choose to remove both breasts after developing breast cancer even without a demonstrated genetic predisposition.
Who cannot have radiation therapy?
Sometimes a woman may be eligible for a lumpectomy, but not for radiation, thus requiring a mastectomy. Not everyone can have radiation therapy. Being pregnant or having certain health conditions can make radiation therapy harmful.
- Pregnancy. Radiation can harm the foetus, so is not given during pregnancy. Depending however on the timing of the pregnancy and the breast cancer diagnosis, a woman may be able to have a lumpectomy and put off radiation therapy until after delivery.
- Scleroderma or systemic lupus. Certain serious connective tissue diseases such as scleroderma or lupus, may make you especially sensitive to the side effects of radiation therapy (In some women at higher risk of breast cancer recurrence, radiation therapy may still be used.)
- Past radiation therapy to the same breast or to the same side of the chest. In general, radiation therapy to the breast can only be given once. (In very rare cases, radiation therapy to the same breast may be repeated after a careful discussion with your radiation oncologist.)

If you have a choice, take time to study your options. In the vast majority of cases there is absolutely no rush to come to a decision, and it is more important that you take your time to come to a decision with which you are comfortable, than to rush into a decision that you may later regret. A short delay before surgery will have no adverse impact on prognosis, and if you feel that your breast surgeon is unduly pressuring you into making a hasty decision, particularly if they indicate that a short delay may influence your prognosis, you may wish to consider a second opinion. See Delay between Diagnosis and Surgery
Weigh up the risks and benefits of each surgical option, and choose the surgery that’s right for you. Survival is the same no matter which option you choose.
It is imperative that all women when choosing their preferred surgical option for early breast cancer are made aware of the fact that the choice of breast surgery does NOT in any way influence the need for or the nature of any post-operative adjuvant systemic (drug) therapy. Whether you will require drug therapies such as chemotherapy, hormone therapy and/or HER2-targeted therapy is based on the characteristics of the breast cancer, including size, grade, nodal and receptor status (hormone receptor and HER2) and not on the type of surgery you have. This is something I cannot emphasise and reinforce enough, choosing more radical surgery, such as mastectomy, does not lessen the chance of chemotherapy being required.
Unlike drug therapy, the need for postoperative radiation IS influenced by the nature of the surgery. Radiation is a local therapy, primarily aimed at reducing the risk of locoregional recurrence within the breast (following lumpectomy), the chest wall (post mastectomy) and the axilla.
Radiation is almost always strongly recommended following breast conserving surgery, and women who indicate preoperatively that they will decline radiotherapy, will often be steered toward mastectomy, as in most cases it is felt that the risk of local recurrence without radiation is unacceptably high. Having a mastectomy does not guarantee that radiation will not be required, but it makes it much less likely. Whether there will be a recommendation for post mastectomy radiation may not be established prior to surgery, as the indications for post mastectomy radiation are pathological factors, such as nodal status, which may not be known until the operative pathology is available. Women who are favouring the option of mastectomy over lumpectomy in the hope of potentially avoiding radiation must therefore be informed preoperatively that undergoing mastectomy is NOT a guarantee that radiation will not be required.
 Reproduced from breastadvocateapp.com
Reproduced from breastadvocateapp.com
Survival and recurrence>
Survival
Survival with lumpectomy (plus radiation therapy) is the same as with mastectomy. Clear margins are also a requirement with lumpectomy (no cancer cells in the tissue surrounding the cancer).
Recurrence
Most people diagnosed with breast cancer will never have a breast cancer recurrence (return of breast cancer). However, everyone who has had breast cancer is at risk of recurrence.
The risk of recurrence varies greatly from person to person. Compared to mastectomy, there’s a slightly higher rate of the cancer returning within the breast (called local recurrence) following lumpectomy. Local recurrence is usually treated with some combination of surgery, radiation therapy, chemotherapy, hormone therapy and/or HER2-targeted therapy.
In large trials where women underwent either a lumpectomy with radiation or a mastectomy, there was no difference in survival—but there was in local recurrence. The rate of breast cancer recurring in the same breast after a mastectomy is usually very low (about 1-3%) and cumulatively perhaps about 10-15% over time after lumpectomy with radiation, but less than 1% per annum.. Importantly, the outcomes in either case are usually good, and most women in both categories will never have to deal with breast cancer again. Women who choose lumpectomy have a slightly higher chance of needing treatment again, but even with mastectomy, the local recurrence rate is not zero.
The risk of cancer spreading to other parts of the body (called metastasis or distant recurrence) is the same following both procedures.

Risks and benefits of mastectomy versus lumpectomy plus radiation therapy
The main benefit of lumpectomy plus radiation therapy is the breast is preserved as much as possible.
A potential benefit of mastectomy is radiation therapy may be avoided. Although some women will need radiation therapy after mastectomy, many will not. (Ask your breast surgeon if you are likely to avoid radiation therapy if you have a mastectomy.)
Radiation therapy has some side effects and requires daily trips to a treatment facility. If you live far away from a radiation treatment centre, or if you cannot have radiation therapy, mastectomy may sometimes be a better option for you than lumpectomy.
The table below outlines some things to consider when choosing between mastectomy and lumpectomy plus radiation therapy.
Total mastectomy versus lumpectomy plus radiation therapy
| Total mastectomy ( +/- immediate reconstruction) |
Lumpectomy plus radiation therapy | |
|---|---|---|
| Treatment for early breast cancer | Very effective | Very effective |
| Amount of breast tissue removed | Entire breast | Part of the breast (tries to retain the original look of the breast) |
| Extent of surgery | More major surgery | Less extensive surgery |
| Hospital stay | Usually 2 night hospital stay (longer if combined with immediate reconstruction) | Usually overnight stay |
| Radiation therapy | Sometimes done | Almost always done |
| Chance of recurrence in the breast (local recurrence) | Very low for early stages of breast cancer | Low for early stages of breast cancer (but slightly higher than with mastectomy |
| Chance of distant metastatic recurrence outside the breast and/or axilla | Same as with lumpectomy plus radiation therapy | Same as with mastectomy |
Deciding factors
Although many women who have a choice, prefer the less invasive lumpectomy, deciding between lumpectomy and mastectomy depends on a how you feel about the following:
- Do you want to keep your breast? If it’s important to you to keep your breast, you may decide to have lumpectomy with radiation instead of mastectomy.
- Do you want your breasts to match as much as possible in size? For most women, lumpectomy has a good cosmetic result. In cases when a larger area of tissue needs to be removed, lumpectomy can cause the breast to look smaller or distorted. A variety of oncoplastic techniques are available if you need to have a larger area of tissue removed. If having two breasts of matching size is important to you, consideration may need to be given to some form of symmetrisation surgery to the opposite “normal” breast (usually a breast reduction or “lift”), either at the time of lumpectomy, or at a later date after radiation to the affected breast.

- How anxious will you be about breast cancer coming back? If removing the entire breast may help you worry less about the possibility of the breast cancer coming back (local recurrence), you might consider mastectomy.
- How much do you fear annual breast screenings and a potential new breast tumour? Many breast cancer patients opt to have a mastectomy – and even a prophylactic mastectomy on the other healthy breast – because they know they’ll feel extreme anxiety during future annual mammograms and over any abnormal finding, follow-up biopsy and possible diagnosis of another breast tumour down the road.
- How much do you want to avoid a painful recuperation? Mastectomy with breast reconstruction typically involves multiple surgical procedures and a potentially uncomfortable/painful healing process that can last for weeks or even months.
- Your general health. Comorbidities such as diabetes, obesity and smoking, significantly elevate the risk of post-operative complications, especially after more major surgical procedures such as mastectomy with immediate reconstruction. Women with comorbidities may be better served undergoing less extensive surgery, such as lumpectomy, in order to avoid a situation in which important post-operative oncological treatment, such as chemotherapy, needs to be delayed because of a post-operative wound complication. See Body Weight and Breast Surgery Complications
- What’s your life expectancy? Women diagnosed with breast cancer at a younger age may be more likely to opt for mastectomy because their longer expected lifespan means they have a higher lifetime risk of recurrence. We typically tell patients that their risk of developing another primary breast cancer is about 0.5 percent per year. A 30-year-old breast cancer patient who expects to live another 50 years may therefore face a 25 percent risk of developing another breast cancer, compared to a 5 percent risk for a woman diagnosed at age 70. Young breast cancer patients are also more likely to carry gene mutations that put them at even greater risk of developing another new primary breast cancer in either breast, which could tip the balance toward having a single or double mastectomy.

Lumpectomy: Advantages and disadvantages
The main advantage of lumpectomy is that it can preserve much of the appearance and sensation of your breast. It is a less invasive surgery, so the recovery time is shorter and easier than with mastectomy.
Lumpectomy has a few potential disadvantages:
- You will almost certainly require radiation therapy, 5 days per week, for 3-6 weeks, after lumpectomy surgery to reduce the chance of the cancer recurring in the breast (local recurrence).
- There is a somewhat higher risk of developing a local recurrence of the cancer after lumpectomy than after mastectomy. However, local recurrence can be treated successfully with mastectomy, and overall survival with lumpectomy and mastectomy are equivalent. While a local recurrence is worrisome, and does require treatment, it may not be fatal, and the vast majority of women who undergo breast conserving surgery will not experience a local recurrence. The real risk to your life is if the cancer spreads to another part of the body. Removing the entire breast does not affect the likelihood of spread to other parts of the body.

- The breast cannot safely tolerate additional radiation if there is a recurrence in the same breast after lumpectomy. This is true for either a recurrence of the same cancer, or for a new cancer. If you have a second cancer in the same breast, your breast surgeon will usually recommend that you have a mastectomy.
- You may need to have one or more additional surgeries after your initial lumpectomy. During lumpectomy, the breast surgeon removes the cancer and some of the normal tissue around it (called the margins). A pathologist looks to see if cancer cells are at the margins. If there are cancer cells at the margins, more tissue needs to be removed, until the margins are free of cancer. Therefore after the pathology report is available, if the margins are found to contain cancer cells, more surgery is required, which may take the form of a margin “re-excision”, excising a small additional piece of breast tissue, or even in some cases, mastectomy.
Mastectomy: Advantages and disadvantages
For some women, removing the entire breast provides greater peace of mind (“just get the whole thing out of there!”). Radiation therapy may still be needed, depending on the results of the pathology.
Mastectomy has some possible disadvantages:
- Mastectomy takes longer and is more extensive than lumpectomy, with more post-surgery side effects and a longer recuperation time.
- Mastectomy means a permanent loss of your breast. and usually loss of sensation in the skin on the chest wall, even if you have a breast reconstruction.

Making your own decision
Your breasts may be such an important part of your identity — your sense of who you are — that you’ll go to great lengths to preserve them. That’s a completely acceptable approach to take, no matter what your age or figure —as long as it doesn’t endanger your overall health and chances for a full recovery.
Over the past decade, women with early-stage breast cancer are increasingly opting for mastectomy or double mastectomy — removal of both breasts. The increased availability of advanced breast reconstruction techniques has contributed to the trend.
Things to consider
There are no right or wrong answers when you are making a decision between treatments. Women each feel very differently. You need to decide what feels best for you.
Some women want to keep their breast if at all possible, so they choose a lumpectomy (wide local excision) and radiotherapy.
Other women feel that once they have breast cancer they would rather have the whole breast removed because it makes them feel it is more likely to remove all of the cancer. They can then choose to have a new breast made (breast reconstruction).
Some women feel strongly that they don’t want radiotherapy. Others welcome it if it means keeping their breast.

Factors affecting which surgery might be best for you:
- the size of your cancer
- where the cancer is in your breast
- whether there is more than one area of cancer
- the size of your breasts
- your general health
What to take into account
To help you decide, you might want to think about:
- how you feel about having the whole breast removed
- how you feel about having only part of the breast removed
- how you feel about having radiotherapy
- how quickly you want the treatment to be finished
- how you would cope with travelling daily for radiotherapy
- whether you would want to have a breast reconstruction after mastectomy
- whether you would want reconstruction straight away or some months after surgery
The most important thing is to take time to find out how you feel and make the right decision for you.
Will having a double mastectomy lower my chances of recurrence?
Regardless of whether you choose to have a lumpectomy or mastectomy, the chance of developing a cancer in the opposite breast is about 0.5 percent per year, and removing the other breast is extremely unlikely to impact on survival, which is almost always related to the original cancer biology and risk of recurrence.
The type of surgery to choose also depends on many other actors, including age, genetic predisposition, gene mutation, extent and location of cancer in the breast, density of breast tissue or the potential anticipated difficulty of imaging surveillance.
Neither surgery has any bearing on whether or not you’ll need chemotherapy
Having more extensive surgery does not mean you can avoid chemotherapy. The need for chemotherapy is determined by how much and what type of cancer is present, as well as your overall health, but NOT by what type of surgery is chosen.
Some choose mastectomy because they fear recurrence, or don’t want the anxiety of continued surveillance screenings. Women should ask themselves “What is my main concern?”
 Reproduced from “I’m Taking Charge”
Reproduced from “I’m Taking Charge”
Helping you to Make the Choice
Patients often get a lot of different information from a lot of different sources around the time of diagnosis, some of which may be unsolicited, and it’s a hard time processing what’s going to be valuable. It’s very difficult when you’re given a cancer diagnosis, “Okay, well what’s going to happen 5, and 10 and 15 years from now?” And how do I make a decision that I’m going to be happy with at that time because right now the only thing that most women are thinking about is that they want to be cured. In addition, it comes at a time that is emotionally charged.

- Clinical Photographs:It is often useful for patients to look at clinical photos to learn what lumpectomies and mastectomies (with or without reconstruction) look like, so that they can understand the reality. Ask your breast surgeon to show you some photos of their own patients.
- Other patients: Talking to other women who have gone through this may also be helpful.
- Decision Aids: A decision aid may also help. Patient decision aids are tools that help people become involved in decision making by making explicit the decision that needs to be made, providing information about the options and outcomes, and by clarifying personal values. They are designed to complement, rather than replace, advice from a health professional. There is good evidence that using decision support tools, such as a patient decision aid, can help consumers by:
- Improving their knowledge of the options
- Helping clarify what matters most to them
- Providing more accurate expectations of possible benefits and harms of their options
- Supporting them to participate more actively in decision making.
For the undecided patient, some will choose BCT if educated about their choices and given proper time for decision-making. Conversely, some women once presented the data and given time to make an informed decision prefer mastectomy. A prospective study of patients eligible for BCT who were provided with a standardized decision support identified 3 treatment outcomes that discriminated between those choosing BCT versus mastectomy. The 3 discriminants were ‘‘remove breast for peace of mind,’’ ‘‘avoid radiation,’’ and ‘‘keep breast.’’
See Decision Aid: Breast Cancer: Should I Have Breast-Conserving Surgery or a Mastectomy for Early-Stage Cancer?
Shared Decision Making and Avoiding Decisional Conflict
The decision confronting early-stage breast cancer patients about surgical treatment options with equivalent overall survival rates, is complex.
Most patients (75-80%) with early-stage breast cancer are clinically eligible for either surgical option, and as such, the decision about the type of surgery is considered ‘‘preference-sensitive’’ because the best choice is dependent on individual patient preference. This can create ‘‘decisional conflict’’, whereby the patient experiences discomfort and doubt as a result of uncertainties in making a preference-sensitive choice. In preference-sensitive decision situations, “decision quality” refers to the extent to which the patient’s choice is (a) informed, (b) consistent with her personal attitudes (ie, her “values”) about the therapeutic options’ pros and cons, and (c) acted on.
Considering three issues has been shown to help both the patient and the physician to come to a decision about the optimal choice for that patient. For the surgery decision, the questions are how interested are you in preserving your breast; how important is peace of mind; and how important is it for you to avoid radiation?
The breast surgeon must be aware of their own personal views and biases to make certain that they are providing the patient thorough knowledge about all of the options. One potential source of decisional conflict for the patient is the potential underlying bias of breast surgeons, many of whom tend to prefer BCT to mastectomy. There is a school of thought amongst many breast surgeons, which I do not personally share, that patients who are suitable for BCT should be advised that BCT is the best treatment option for them, and that not only does it confer at least equivalent survival, but that compared with mastectomy, it has the advantages of fewer complications, better quality of life and many less operations, if reconstructive surgery is performed. These surgeons state that “it may no longer be appropriate to offer women suitable for BCT the choice of mastectomy or BCT.” (5) One study which suggested that surgeons strongly favoured BCS, found that nearly one fifth of patients reported that their surgeon only described BCS, whereas only approximately 3.5% of women reported that their surgeon only described mastectomy. (9)

This is an approach with which I strongly disagree. Having explained to a patient that survival is equivalent between BCS and mastectomy, and reassuring them that we would never offer the choice between two options if one was clearly superior, it seems very paternalistic to me to then only offer or strongly recommend one of the options over the other. Sure there may be times when a patient comes to a decision which I may not necessarily share, for example chooses mastectomy over BCS for a small, impalpable screen detected cancer less than 1cm in size, but that is the whole basis of “personal preference-sensitive “decisions. They are based on the patient’s personal preference, not on the breast surgeon’s, and although conventional wisdom may view BCS as the preferred treatment, a notable proportion of well informed women will in fact choose mastectomy.
In a population-based study of 1844 women, 41 % reported that they made the surgical treatment decision, 37 % reported that it was a shared decision with their surgeon, and 22 % reported that the surgeon made the surgical treatment decision. Only 5 % of patients whose surgeon made the treatment decision underwent mastectomy, compared with 17 % when a shared decision was made, and 27 % when the patient made the treatment decision, the data suggesting that increasing patient involvement increases rather than decreases mastectomy rates. (9)
My role as a breast surgeon is to ensure that the patient is fully informed of the surgical options, their relative merits and disadvantages, and is given adequate time to come to a considered decision. As long as I am satisfied that the decision has not been based on an incorrect assumption, such as that “undergoing mastectomy will improve my survival”, I should accept the patient’s choice. It is not appropriate to offer the patient the choice between two options, only to then refuse to accept their decision. An exception to this would however be the situation in which the patient requests a surgical option which is not in her best interests medically, usually because of comorbidities. One example would be the obese, diabetic, smoker who is suitable for BCS, but requests bilateral mastectomy with immediate reconstruction.

In some situations, despite being fully informed and given adequate time, the patient truly cannot come to a decision, and my default is then to advise the less radical option of BCS. Sometimes a patient’s decision making can be literally “paralysed” by the fear and uncertainty created by the recent cancer diagnosis, and once the lumpectomy surgery is complete and pathology available, the situation becomes less stressful for them, and decision making clearer. If having undergone BCS, the patient then decides that they would prefer mastectomy, that can always be performed subsequently, often after chemotherapy is completed. This approach, although uncommonly required, also allows the stressed/undecided patient to be rid of the cancer, and then be able to concentrate on non-oncological decisions such as breast reconstructive options, in a less stressed state of mind.
Treatment decision making in oncology can be complicated, and patients may look to clinicians to navigate these uncertain waters, because they may not have the desire or expectation to control or share in all treatment decisions. There are many challenges to shared decision making with patients. The diagnosis of cancer is a stressful experience for most patients. They and their families must make many treatment decisions with limited knowledge and major consequences over a short period of time. Most of these decisions are made with clinicians they have met for the first time under difficult circumstances.
Mastectomy vs Lumpectomy
Videos
- Breast Conserving Surgery, Lumpectomy or Wide Local Excision
- Mastectomy
- Making Treatment Choices for Breast Cancer
Websites
- Choosing between breast conserving surgery or mastectomy
- Mastectomy vs. Lumpectomy
- Choosing surgical treatment for early-stage breast cancer
- Deciding Between Mastectomy or Lumpectomy
- Lumpectomy vs. Mastectomy 1
- Lumpectomy vs. mastectomy 2
Resources/References
Should I have a lumpectomy or mastectomy?
How do I choose between a mastectomy and lumpectomy
When Informed, All Women Do Not Prefer Breast Conservation. 2009
Can Women With Early-Stage Breast Cancer Make an Informed Decision for Mastectomy? 2009
Patient Involvement in Surgery Treatment Decisions for Breast Cancer. 2005
Patient choice significantly affects mastectomy rates in the treatment of breast cancer .2008