Types of Breast Reconstruction including Direct-to-Implant (DTI) & Acellular Dermal Matrix (ADM)
There are three main types of breast reconstruction:
- Implant based
- Autologous or ‘tissue flap’ reconstruction -where your own tissue is used
- A combination of both.
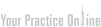
Breast reconstruction is commonly performed in several stages: restoration of the breast contour, revisions, and reconstruction of the nipple-areolar complex or increasingly these days in one stage, with nipple-sparing mastectomy and immediate autologous reconstruction or direct-to-implant (DTI) reconstruction with an acellular dermal matrix (ADM).
The choice of technique is influenced by several factors:
- your preference
- your body shape, build and breast size
- your general health, including importantly, whether you smoke
- the amount of tissue that has already been removed
- scars from previous operations
- the quality of the remaining skin
- the breast size you would like
- whether you need radiotherapy or have already had it
Implant Based Breast Reconstruction (IBBR)
Implants are often used to reconstruct a breast following mastectomy.
There are 2 types of breast reconstruction options using implants only:
- Tissue Expander/ Implant Reconstruction (Two Stage)
- Direct-to-Implant (DTI) (One Stage) Reconstruction with Acellular Dermal Matrix (ADM)
Patient selection is an important factor when considering prosthetic reconstruction, as a 1 or 2 stage technique. Poor candidates for prosthetic reconstruction often include women that have had prior radiation therapy, morbidly obese patients, and patient that are actively smoking tobacco products. The decision regarding skin vs. nipple sparing mastectomy is dependent on patient selection, with larger volumes usually having skin-sparing techniques.

1. Tissue Expander/ Implant Reconstruction (Two Stage)
This is the more traditional approach, and is still the most commonly performed technique in Australia. In the first stage of this procedure, a tissue expander is inserted into a pocket created under your skin and chest muscle. The tissue expander is a silicone balloon filled with saline (sterile salt water). The expander is partially inflated with saline after insertion, whilst you are asleep. Following the initial operation, and over a period of weeks to months, a valve in the expander allows the surgeon or nurse to inject further saline solution and gradually fill the expander to help stretch the muscle and skin to the breast size desired. After the skin over the breast has been fully stretched to achieve the desired size and allow for placement of the permanent implant, a second operation is undertaken to exchange the tissue expander for a permanent implant.



Anatomical tissue-expander with integral filling port
Implants are categorized by their filler substance (silicone vs saline), surface (textured vs smooth), shape (round vs anatomic), and size. Implant-based breast reconstructions are best suited to women with small to medium breasts, minimal ptosis (sag) and healthy mastectomy flaps, and those undergoing bilateral mastectomies. Patients with potentially unfavorable outcomes include: obese women with large breasts, smokers, and patients with prior breast radiotherapy.
![]()
![]()
Silicone Implants
2008 US figures showed that approximately 60% of immediate reconstructions were implant based compared with 40% autologous, which was a reversal of previous findings. Although the reason for the increase in implant use is multifactorial, a change in mastectomy patterns, such as increased use of bilateral mastectomies, is one important contributor. In addition, as women younger than 49 years represented an increasing portion of the patients undergoing
reconstruction, and had higher reconstruction rates than older women, it has been conjectured that these younger patients may prefer implant-based reconstruction because they less commonly have adequate tissue available to permit autologous reconstruction, or may prefer to avoid the potentially extended recovery and donor-site morbidity.
2. Direct-to-Implant (DTI) (One Stage) Reconstruction with Acellular Dermal Matrix (ADM)
This is a newer technique that is not yet widely available in Australia. Direct-to-Implant (DTI) breast reconstruction is an alternative approach to the traditional expander-implant breast reconstruction. It allows the placement of a breast implant right after a mastectomy is completed, in one operation.
Jane O’Brien and her plastic surgical colleagues have extensive experience with this new technique, and use it frequently in carefully selected patients. In 2016, 83% of the immediate implant-based reconstructions we performed on women undergoing mastectomies for cancer were one stage, direct-to-implant (DTI). 100% of the women undergoing bilateral risk reduction mastectomy in 2016 underwent bilateral nipple-sparing mastectomy with immediate one stage direct-to-implant (DTI) reconstruction.

This procedure is suitable for selected women who are having nipple-sparing (or skin-sparing) mastectomies and are seeking immediate reconstruction. The technique aims to provide one-step surgery through the use of a specialised surgical mesh (biological Acellular Dermal Matrix (ADM) or prosthetic mesh eg Titanium-coated polypropylene mesh- TiLoop®) to create a sling within the chest that cradles the implant, which is inserted at the same time.
A biological mesh—also referred to as an acellular dermal matrix (ADM)—is a scaffold of dermis produced from cadaveric human (FlexHD®, Alloderm®, Allomax®, DermaCell®), porcine (Strattice®, PermacolTM), bovine (SurgiMend®), or bovine pericardium (Veritas®) tissue that has been specially treated and is stripped of its antigenic cells through specialised processing, and has been approved for use in this type of procedure.
As the surgeon can manipulate the implant position within the sling the result is a more natural looking breast. The ADM looks like very thin white leather (pictured below) and provides a ‘hammock’ that cradles the breast implant, helping to create a natural droop, shape and contour.


The mesh is attached to the pectoralis muscle in the chest making a cavity in which the implant can be placed, especially in cases of nipple-sparing mastectomy. By attaching to the inferior-lateral pole of the muscle, the mesh expands the space available for the insertion of an implant, filling the void left between the muscle and fascia, thereby creating a natural inframammary fold. This tech- nique provides additional cover and support inferiorly, enabling faster tissue expansion, larger implant volumes, and improvement of lower pole projection.

- Nipple-sparing mastectomy (NSM) via inferolateral inframammary incision. The muscle is released to approximately the 4 or 8 o’clock position on the chest wall to allow medial implant positioning and partial muscle coverage.

- The pectoralis major muscle is released from its inferior attachment An acellular dermal matrix or mesh is used to recreate the inferior and lateral boundaries for the implant, and to create a complete pocket around the implant with the pectoralis muscle.

- The implant is placed into the submuscular-subADM pocket

By off-loading stress on the inferior skin envelope, and by changing the interface of the skin envelope with the implant, it is thought that ADM-assisted reconstruction may also be associated with lower contracture rates than reconstructions without ADM.

The technique of one-stage direct-to-implant reconstruction with acellular dermal matrix has expanded the surgeon’s repertoire and given carefully selected patients an opportunity to have a one-stage option in conjunction with nipple-sparing mastectomy (NSM).

There are no widely accepted criteria that need to be fulfilled in order for NSM to be performed; however, several factors are considered for each potential candidate. Potential contraindications to NSM include smoking history, larger breast size, and ptosis. In breast cancer patients, those with skin or nipple involvement, central tumours close to the NAC, or blood stained nipple discharge are generally considered unsuitable candidates for NSM. All patients undergoing NSM meet with a breast surgeon and a plastic surgeon with a special interest in breast reconstruction preoperatively, to discuss the risks and benefits of NSM compared to skin-sparing mastectomy, both oncologically and aesthetically.
The option of nipple-sparing mastectomy with DTI reconstruction is particularly attractive to younger women with a genetic disposition to breast cancer, undergoing bilateral risk reduction mastectomy.



Acellular Dermal Matrices are increasingly being used worldwide to provide inferolateral implant or tissue expander coverage at the breast lower pole in implant-based breast reconstruction. According to a US survey, greater than 50% of American Society of Plastic Surgeons who predominantly perform implant based reconstructions use ADM. Ann Plast Surg, 2011. The use of an acellular dermal matrix does however incur additional costs and may be associated with higher risks of complications compared with tissue expander placement alone. Notwithstanding their utility and importance, ADMs have shown, not always at a statistically significant level, a trend toward a higher complication rate when compared to standard whole muscular pocket implant reconstruction, particularly infections and seroma.
If you are interested in exploring whether the option of a reconstruction incorporating the use of a mesh or ADM is something that may be considered in your case, you should check as to whether your particular treatment team has experience in its use.
If you are interested in exploring whether the option of a reconstruction incorporating the use of a mesh or ADM is something that may be considered in your case, you should check as to whether your particular treatment team has experience in its use.
Patient selection begins at the initial consultation. The history assesses the overall health of the patient and treatment plan, previous surgeries and co-morbidities, current medications, and smoking status. The ideal candidate for DTI reconstruction is an otherwise healthy non-smoker with a small to moderate sized breast, and who desires to be a similar breast size.

If a patient wishes to be signicantly larger in size, this is typically more safely done in two stages with tissue expander-implant reconstruction. Patients who have multiple medical co-morbidities that increase the complication risk may be better served with delayed reconstruction. Active smoking and pre-existing scars on the breast adversely affect skin perfusion and thus DTI may not be possible. The skin of the large breast may also pose challenges as it tends to become more ischemic than the skin of smaller breasts with mastectomy. Therefore, even though there is often an excess amount of skin available to use, reconstruction may need to be done in two stages or it may even need to be delayed. If the patient meets the above criteria, she is a candidate for DTI reconstruction. However, the final decision on DTI is made in the operating room based on the health and perfusion of the mastectomy skin envelope, and the surgeon should be prepared to do a tissue expander reconstruction if required. By limiting the volume of the tissue expander at the initial operation such that the skin envelope is expanded but not under tension, the risk of mastectomy skin flap and nipple-areolar ischaemia is reduced.
The decision to proceed with immediate one-stage or two-stage breast reconstruction depends on multiple factors related to the patient, disease, and treatment. Perfusion to the skin and nipple comes primarily from the breast that must be removed. Thin mastectomy flaps are desirable from an oncological standpoint because leaving fibroglandular tissue behind poses an oncological risk, but the risk of damage to the subdermal vascular plexus, the only remaining source of skin perfusion after mastectomy, is increased, and damage can result in the remaining skin becoming ischaemic and can hinder healing after mastectomy.

Those commonly believed to be the best candidates for one-stage implant reconstruction: young, thin women, with no pre-existing medical comorbidities or history of smoking, who desire reconstructions similar to or smaller than their original breast size.
Although the idea of having everything taken care of in one operation sounds great, and the DTI procedure can be a great option for some women, calling it “one and done” as it is commonly referred to in the USA, can be misleading, as over 30% of women will need further revisional surgery. The main advantage of direct-to-implant breast reconstruction is the elimination of the lengthy, inconvenient and occasionally poorly tolerated tissue expansion process, which can be uncomfortable and requires multiple office visits.
Reconstruction with Your Own Tissue (Autologous Tissue)
With autologous reconstruction, the breast is made from areas of the patient’s body where there is “excess” tissue, such as the stomach, the back, the buttocks, or even the thigh. The tissue is then moved to the mastectomy area and shaped to form a new breast.

Autologous breast reconstruction permits creation of ptosis and the transferred tissue adjusts to changes in body weight. Autologous reconstruction is divided into two large groups: pedicled and free flaps. Pedicled flaps rely on their native blood supply and free tissue transfers require complete severance of existing blood vessels and microvascular reconstruction of these in their new positions. In general, these procedures are more complex than implant based breast reconstruction. Breast reconstruction with your own tissue is an excellent option for women who wish to avoid the use of implants.

Animation: Immediate DIEP Flap at the time of skin-sparing mastectomy
Reconstruction with Your Own Tissue and Implants
Sometimes a combination of techniques is needed for reconstruction. In such cases an implant, along with for example back muscle (latissimus dorsi) and skin can be used to create the breast.
Nipple and Areola Reconstruction
For women undergoing skin-sparing mastectomy, in which the nipple/areolar complex is removed, after the breast mound is made, many women choose to have the nipple and the areola reconstructed at a later date. There are many techniques available for nipple reconstruction. Most involve using local breast tissue to create a small mound about the same size as the other nipple. An areola can be created using a tattoo treatment to dye the skin which is done as an office procedure.

The remaining breast
For many women, the small difference between their remaining and reconstructed breast is not noticeable when they wear a bra. For others, the difference in breast size may be quite noticeable. Some women decide to have the remaining breast made smaller through surgical breast reduction, or lifted (mastopexy procedure) either at the time of initial reconstruction, or later, as a delayed procedure. Others may choose to enlarge and lift the remaining breast to match the other side.

Right breast reduction for symmetry after left breast reconstruction (left nipple reconstruction at the same time).

Right breast augmentation for symmetry after left breast reconstruction (left nipple reconstruction at the same time).
It is important that your breast reconstructive surgeon is experienced and knowledgeable in all the techniques of breast reconstruction. While all surgeons are biased by their training and experience, it is probably best to avoid a surgeon who utilizes the same reconstructive technique for all patients. As it is the breast surgeon who usually serves as the point of initial contact in the treatment of breast cancer, he/she acts as the gatekeeper to the rest of your treatment team and your onward referrals to all the other specialists including the plastic surgeon, are determined to a large extent by your choice of breast surgeon. This again underlines and reinforces the importance of your initial decision in choosing your breast surgeon.
Breast Prostheses Reconstruction booklet
Breast Reconstruction for Breast Cancer Patients
BAPRAS Your Guide to Breast Reconstruction
For further resources on Breast Reconstruction see Breast Reconstruction Information Resources